
Our Office
3125 Coffee Rd.
Suite 1
Modesto, CA 95355
Existing Patients: (209) 529-2726
New Patients: (209) 207-5740
Visit Us Online

Wisdom teeth, also known as third molars, are the last set that typically emerges at the back of the mouth during late adolescence or early adulthood. While some wisdom teeth come in without causing any problems, others may experience issues requiring extraction. At Wayne T. Yee, DDS, wisdom teeth extractions are a standard dental procedure to remove these molars and prevent potential complications.
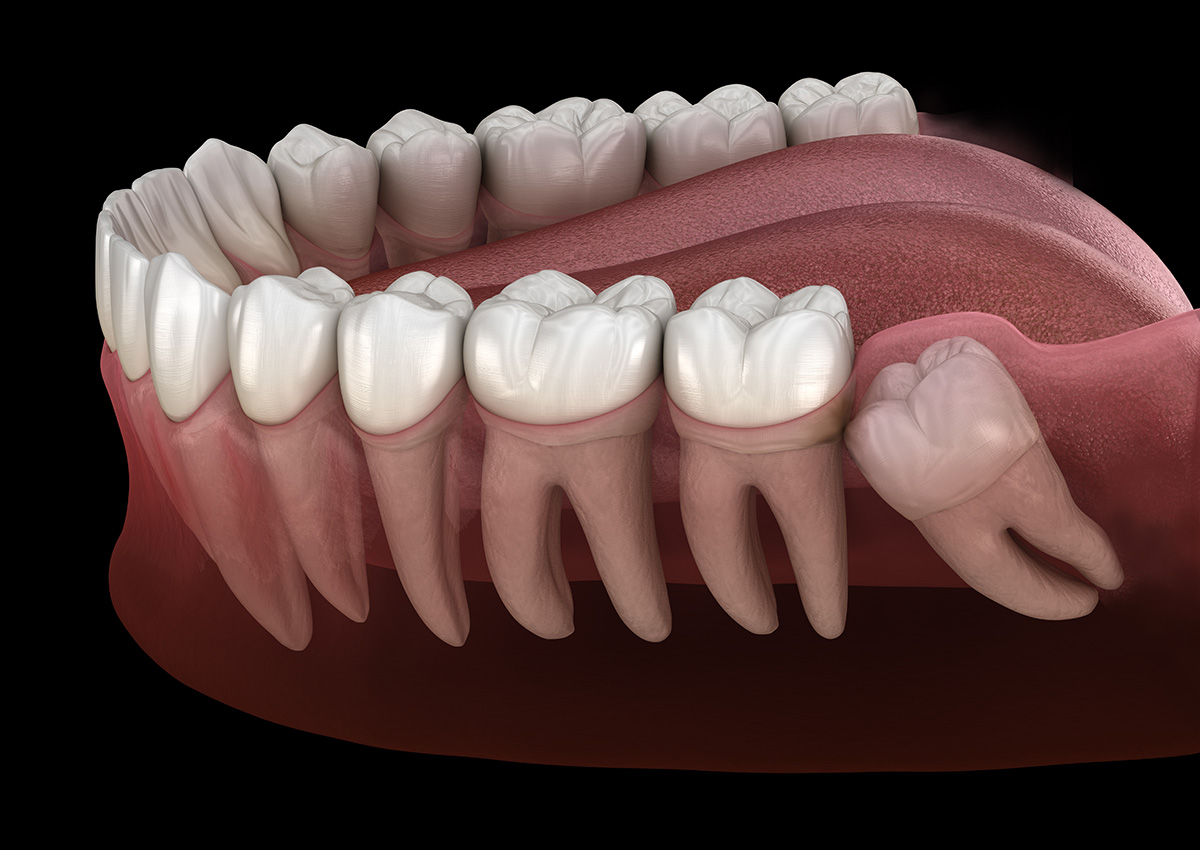
The most common reason for wisdom teeth extractions is insufficient space in the mouth. When there is not enough room for the wisdom teeth to emerge properly, they may become impacted, meaning they cannot fully break through the gum line. Impacted wisdom teeth can lead to various issues, including pain, infection, and damage to neighboring teeth.
Wisdom teeth may erupt at awkward angles or positions, causing them to press against neighboring teeth. This misalignment can result in crowding and disrupt the alignment of your existing teeth.
A fluid-filled sac may sometimes form around the impacted wisdom tooth, resulting in a cyst. Cysts can damage the surrounding bone and teeth and require surgical removal.
Wisdom teeth are located at the back of the mouth, making them difficult to clean properly. Poor oral hygiene can lead to tooth decay and gum disease in these molars and neighboring teeth.

Before the extraction, you will be given local anesthesia to numb the area around the wisdom tooth. Sometimes, conscious sedation or general anesthesia may be used for more complex extractions or to help anxious patients feel more comfortable. The dentist or oral surgeon will make an incision in the gum tissue to access the wisdom tooth during the extraction. If the tooth is impacted, a portion of bone may need to be removed to access the tooth entirely. The wisdom tooth will then be carefully extracted from the socket.
Once the tooth is removed, the area may be stitched to promote healing. A gauze will be placed over the extraction site to control bleeding and facilitate blood clot formation. After the extraction, you will be provided with aftercare instructions. It is essential to follow these instructions to ensure a smooth and speedy recovery.
Wisdom teeth extractions are a standard dental procedure that can prevent potential complications and maintain oral health. Extraction is often the best course of action when wisdom teeth are impacted, misaligned, or causing other dental issues. If you suspect that your wisdom teeth may be causing problems, contact Wayne T. Yee, DDS, at 3125 Coffee Rd # 1, Modesto, CA 95355, or call (209) 529-2726.
Wisdom teeth, also called third molars, are the last permanent teeth to develop and typically emerge in the late teens to early twenties. They can erupt normally in some patients, but many people have jaws that are too small to accommodate these additional molars. When wisdom teeth cannot erupt fully or come in at an awkward angle, they may become impacted and create pressure on surrounding structures.
Impacted or poorly positioned wisdom teeth increase the risk of pain, infection, decay, gum disease and cyst formation around the affected tooth. Extraction is often recommended to prevent these problems or to address them if they are already present. Your dentist evaluates the tooth position and overall oral health to determine the best approach for each patient.
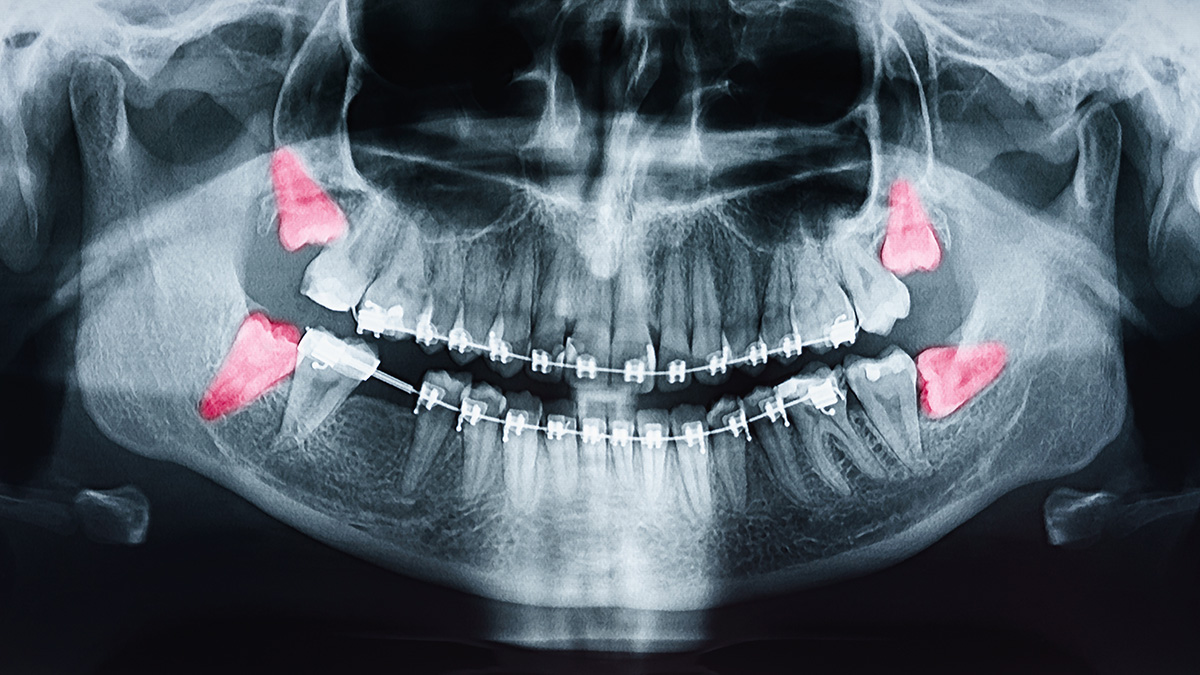
Routine evaluation of wisdom teeth usually begins in the late teenage years or early twenties, when third molars are developing and their path of eruption can be assessed. A clinical exam combined with a panoramic X-ray or other imaging helps your dentist determine whether there is enough space and whether the teeth are likely to erupt normally. Early evaluation allows the dental team to monitor development and recommend timely intervention if problems are anticipated.
You should seek an exam sooner if you experience symptoms such as persistent pain at the back of the mouth, swelling, recurrent infections, difficulty opening the mouth, or sudden changes in the bite. Prompt assessment can limit complications and make management more predictable. Your dental team will explain the findings and outline monitoring or treatment options tailored to your needs.
Decision-making begins with a thorough clinical exam and diagnostic imaging to evaluate tooth position, root formation, proximity to nerves and sinuses, and the health of adjacent teeth and bone. The dentist will assess whether a wisdom tooth is fully erupted, partially erupted, impacted, decayed, or associated with gum problems or cysts. These factors, plus the patient’s age, medical history and symptoms, guide the recommendation for extraction or observation.
Not all wisdom teeth require removal; some can be safely monitored over time with periodic exams and imaging. When extraction is advisable, the dental team will explain the expected benefits and choice of treatment, which may include a referral to an oral surgeon for complex cases. A personalized treatment plan helps ensure the safest and most effective outcome.
On the day of the procedure the dental team will review your medical history and confirm the chosen anesthesia or sedation option. For an impacted tooth the dentist or surgeon makes a small incision in the gum to access the tooth, and may remove a small amount of bone or section the tooth to facilitate safe removal. Local anesthesia, sedation or general anesthesia is used as appropriate to keep the patient comfortable throughout the process.
After the tooth is removed the site may be smoothed and sutured to promote healing, and gauze is placed to support clot formation. You will receive clear aftercare instructions covering pain management, oral hygiene and activity restrictions to protect the healing site. The team schedules follow-up as needed to monitor healing and address any concerns.
Several anesthesia and sedation options may be offered depending on the complexity of the extraction and the patient’s level of anxiety and medical history. Local anesthesia numbs the area around the tooth, while nitrous oxide, oral sedatives or intravenous (IV) sedation provide varying levels of relaxation and reduced awareness. In select cases or for extensive procedures, general anesthesia may be used so the patient is fully unconscious for the duration of treatment.
Your dentist or oral surgeon will discuss the risks and benefits of each option and recommend one based on the procedure and your overall health. Pre-procedure instructions and monitoring during treatment help ensure safety and comfort. Always disclose all medications and medical conditions so the team can tailor anesthesia planning appropriately.
Initial recovery typically involves a period of localized swelling, mild bleeding and controlled discomfort during the first few days after extraction. Pain is usually managed with prescribed or over-the-counter medications and by using cold packs to minimize swelling during the first 24 to 48 hours. Rest and limited physical activity help the body focus on healing, and most patients notice steady improvement within a week.
Diet should focus on soft, nutritious foods and adequate hydration while avoiding actions that could dislodge the blood clot, such as using straws or vigorous rinsing. Maintain gentle oral hygiene around the surgical site as instructed, and attend any scheduled follow-up appointments so your dentist can confirm proper healing. Contact your dental team promptly if you experience severe pain, heavy bleeding or other concerning symptoms.
Common complications after extraction may include pain, swelling, bleeding and transient difficulty opening the jaw, all of which are typically managed with home care and follow-up support. More specific concerns include dry socket (alveolar osteitis), postoperative infection, nerve irritation or injury and, in rare cases, sinus communication when upper molars are involved. The dental team monitors for these outcomes and provides timely treatment when they occur.
Management can include in-office cleaning and medicated dressings for dry socket, antibiotics for infections when indicated, and additional interventions for rare complications. Because nerve-related symptoms require careful assessment, persistent numbness or altered sensation should be reported immediately. Your dentist will explain signs to watch for and the steps to take if a problem arises.
Protecting the blood clot that forms in the extraction site is the most important measure to reduce the risk of dry socket. Avoid smoking and tobacco use before and after surgery, refrain from using straws or performing strong suction, and follow all postoperative instructions regarding oral hygiene and activity level. Gentle rinsing with warm salt water is usually recommended after the first 24 hours, but aggressive spitting or rinsing should be avoided during the earliest healing phase.
Following medication guidance and attending follow-up visits also help the dental team identify and address any early signs of complications. If severe or worsening pain develops several days after surgery, contact your dentist promptly so the site can be evaluated and treated. Early intervention limits discomfort and supports uncomplicated healing.
Impacted wisdom teeth can exert pressure on neighboring molars, increase the risk of decay and periodontal problems in adjacent teeth, and in some cases contribute to root resorption or localized bone loss. These issues can complicate long-term dental health and may jeopardize the stability of nearby teeth. During orthodontic treatment, the presence of impacted third molars is evaluated to determine whether removal would benefit overall treatment goals and long-term alignment.
Decisions about extraction in the context of orthodontics are individualized and often made in collaboration with the orthodontist and the dentist or oral surgeon. The care team will consider timing, the position of the wisdom teeth, and the status of the patient’s bite before recommending monitoring or removal. Clear communication between providers ensures treatment plans support lasting oral health and function.
You can schedule a consultation by calling the office at (209) 529-2726 for existing patients or (209) 207-5740 for new patients, or by requesting an appointment through the practice’s appointment channels. During the consultation the dental team will review your medical and dental history, perform an exam and obtain any necessary imaging to assess the wisdom teeth and create a personalized treatment plan. The visit is an opportunity to discuss anesthesia options, expected recovery and any questions you may have.
Bring a list of current medications, any relevant medical records, and your insurance card if applicable to help the team coordinate care efficiently. The office of Wayne T. Yee, DDS will provide clear preoperative instructions if extraction is recommended and will arrange a follow-up plan to monitor healing. If you have concerns about anxiety or medical conditions, mention them at the time of scheduling so the staff can prepare appropriately.
